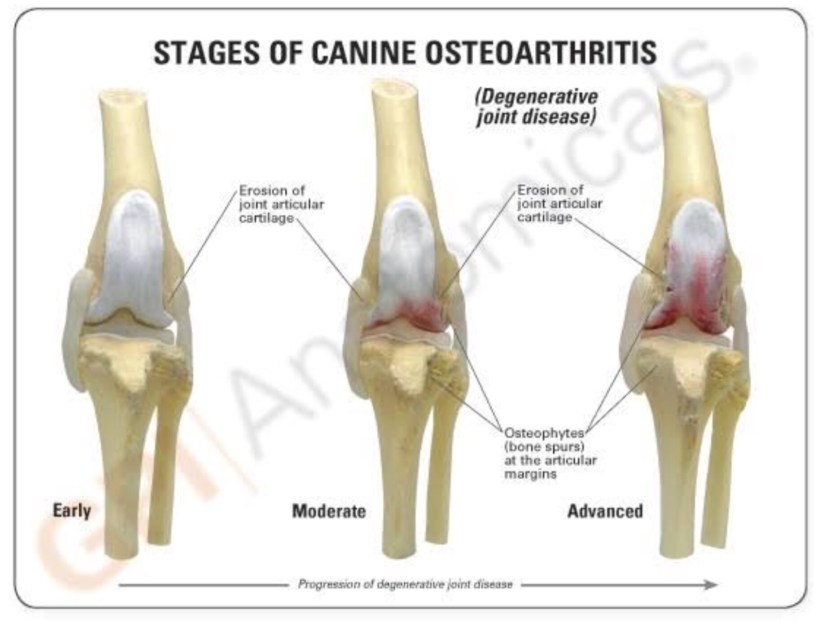
Osteoarthritis (OA), aka degenerative joint disease, is a slow progressive inflammatory disease of joints characterised by degradation of the cartilage, thickening of bone margins, and changes in the synovial membrane. The end result of this process is painful and stiffen joints. Unfortunately it cannot be cured, but managed and usually involves a multimodal approach.
OA can affect any joint of any breed of dog and cat, even though large and giant breed dogs are the most commonly thought of when OA comes to mind. Common clinical signs of OA noticed by owners are usually: pain and stiffness while the animal is running, walking, jumping, or rising from a lying or sitting position; reluctance to walk and jump, lameness, favouring limb and aggressiveness.
Examination of the pet includes observation of the pet walking/running from a distance and complete orthopaedic exam in which the affected joints are checked for alignment, range of motions, presence or absence of pain inflammation, swelling, or crepitus. A neurologic exam is also performed assessing the patient’s conformation, balance, gait, muscle loss.
The next step in investigating OA involves imaging of the affected joints. The most common is radiography. Radiographs are usually done under sedation or general anaesthetic and they can reveal calcification within and around the joint, often appearing as new bony formations called osteophytes. Another diagnostic tool is arthroscopy, a minimally invasive procedure that allows you to see changes in the joint before they become apparent in radiographs. It is also used as a therapeutic procedure (allows removal of loose fragment of bone, cartilage and ligaments) and it requires a general anaesthetic.
The management of OA is aimed at minimising joint pain by reducing the inflammation and slowing the progression of cartilage damage, therefore promoting an increase in joint flexibility and quality of life. For this, the multimodal management approach relies on medical and non medical management. Medical management relies on use of nonsteroidal anti-inflammatory drugs (NSAIDs), chondroprotectants and adjuncts (opioids, tramadol, steroids, gabapentin, pentosan, for example); while the non medical management includes weight control/exercise, EPA-rich diet and physical rehabilitation.
It is also worth mentioning that sometimes surgery will be necessary to stabilise the joint prior to medical treatment.
Before starting treatment for OA it is important to perform blood work and a urine test (urinalysis) to rule out kidney disease as some of the medications for OA can be deleterious to the kidneys.
Have you noticed that your pet has been slowing down or seems stiffer than usual? Call 0423 600 618 and book an appointment with Dr Pat the Vet to have him checked over.